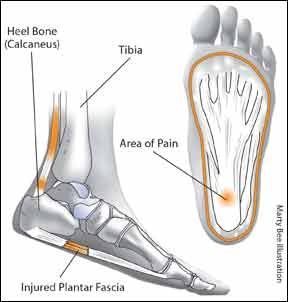
If you experience severe heel pain, chances are you have plantar fasciitis. For foot and ankle specialist Brian Donley, MD, President of the Cleveland Clinic-affiliated Lutheran Hospital and Editor-in-Chief of Arthritis Advisor, plantar fasciitis is one of the most common diagnoses in his clinic. And, this frustrating condition can linger for weeks or months. "It can be very debilitating, he says. Its almost epidemic, and it happens in all types of people. In most cases, plantar fasciitis and other causes of heel pain can be addressed without the need for surgery. The key is to pinpoint the source of the pain and use simple treatments to get back in step.
To continue reading this article or issue you must be a paid subscriber.
Sign in