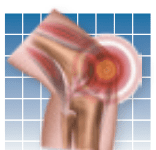
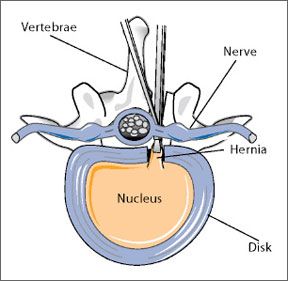
If youve ever endured a backache, youre not alone. Back pain plagues eight out of 10 Americans at some point in their lives. In older adults, back pain typically stems from one or more of four sources: wear and tear of spinal joints due to arthritis; degenerated or herniated disk; fractured vertebrae due to osteoporosis; or soft tissue problems involving ligaments, tendons, or the muscles that support, operate, and stabilize the spine. Conservative treatment involves medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen, or celebrex; physical therapy; and exercise. Some patients try chiropractic manipulation, acupuncture, and massage therapy. Other means of physical support such as bracing, orthotics, and canes may also ease pain. But medications can have side effects, and many treatments offer only temporary relief. Surgery, often a last resort, can be risky.
To continue reading this article or issue you must be a paid subscriber.
Sign in