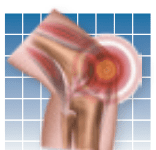
The treatment of psoriatic arthritis-a chronic disease that causes a scaly, itchy skin rash on the elbows, knees, and scalp-advanced significantly late last year when experts published the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) in the September 2009 issue of Annals of the Rheumatic Diseases. "This evidence-based guideline categorizes psoriatic arthritis based on the predominant symptoms, and provides a step-wise approach to treatment," says Elaine Husni, MD, MPH, vice chair of the Department of Rheumatology and director of the Arthritis and Musculoskeletal Center at Cleveland Clinic.
To continue reading this article or issue you must be a paid subscriber.
Sign in