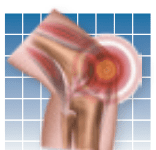
Pain is the main reason people with osteoarthritis seek medical care. A study published in
Arthritis Care & Research (August 2018) found that insomnia and depression were also significant reasons for going to a doctor. Painful arthritis can lead to sleep problems and depression, and having these conditions can worsen pain. The researchers analyzed health records of close to 3,000 participants in a health plan who had been diagnosed with osteoarthritis. Close to half of them reported pain that was moderate to severe. About 34 percent of all participants had insomnia in addition to moderate to severe pain, and 29 percent had depression along with pain. Pain was the main driver for seeking medical attention. But the combined effects of pain plus insomnia and pain plus depression increased the likelihood of seeing a healthcare professional, and this increased with the severity of these conditions.
To continue reading this article or issue you must be a paid subscriber.
Sign in