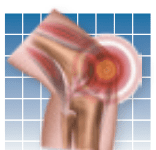
Hip arthritis is usually experienced as pain in the groin. It can also cause pain on the front of the thigh or even pain around the knee. Having achy joints can be frustrating. It may seem logical that resting the joint will help. But, in fact, the opposite is true. Joints are meant to move, and they need movement to be healthy. The mobile joints in the body are lined with a membrane that secretes synovial fluid, which provides nutrition and lubrication. Some form of compression (from walking or other physical activity) is needed to circulate the nourishing synovial fluid across the joint.
To continue reading this article or issue you must be a paid subscriber.
Sign in