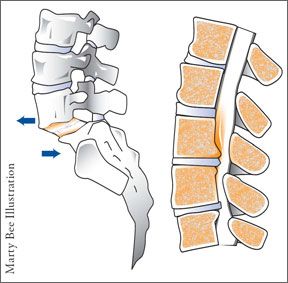
When is it appropriate to forego non-surgical treatment and spring for surgery for back pain? According to a study published in the June 2009 Journal of Bone and Joint Surgery, patients with spinal stenosis (narrowing of the spinal canal, causing nerve compression) and degenerative spondylolisthesis (a slipped disk, usually due to arthritis) who chose to have surgery had substantially greater pain relief compared with those who did not choose surgery. The patients who had surgery also had better function, less pain, and higher satisfaction two and four years later compared with those who chose not to have surgery.
To continue reading this article or issue you must be a paid subscriber.
Sign in