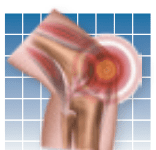
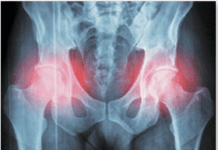
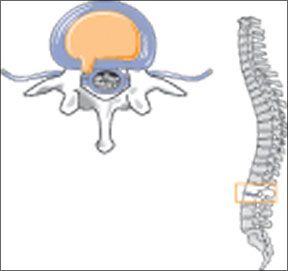
Whether you call it a ruptured disk, herniated disk, or lumbar disk disease (LDD), the result is pain. This age-related condition develops when the jelly-like material inside the shock-absorbing disks of your spine pushes out of its normal space, placing pressure on spinal nerve roots. For some, the low-back pain is especially intense when they cough, sneeze, sit, twist, or stand in the same position for a prolonged period of time. For others, it is pain that begins in the lower back or buttocks and radiates down the back of one leg (sciatica). For still others, a ruptured disk can cause muscle spasms in the back, weakness or numbness in the leg or foot, and even changes in bladder and bowel function. Surgery would seem to be a logical solution for such a debilitating condition-but its a last resort, not a first choice. "Without treatment," says A. J. Cianflocco, MD, staff physician at Cleveland Clinics Sports Health Center, "60 percent of patients get better. With treatment, up to 95 percent improve without surgery. Depending on age, severity of the condition, expectations, and preferences, a patient can choose from a variety of non-invasive or minimally invasive procedures, starting with activity modification and relative rest."
To continue reading this article or issue you must be a paid subscriber.
Sign in