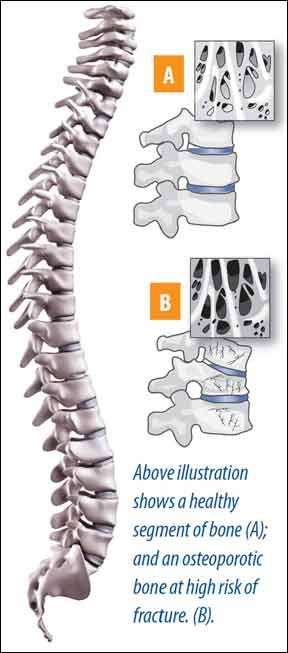
The popular bone-building drugs called bisphosphonates are known for their powerful impact on regaining bone density and reducing fractures. Yet, recent headlines have questioned the long-term efficacy and safety of bisphosphonates in women who take them, causing many to wonder if the drugs benefits are worth the risk.Since the U.S. Food and Drug Administration (FDA) raised concerns in 2011 about the potential for serious side effects in women taking bisphosphonates, including alenodrate (Fosamax), risedronate (Actonel), zoledronic acid (Reclast) and ibandronate (Boniva), both physicians and their patients have been on alert.
To continue reading this article or issue you must be a paid subscriber.
Sign in