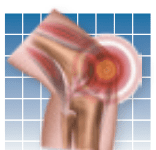
A diagnosis of rheumatoid arthritis (RA) is not as disabling as it was 20 years ago, researchers reported online in Arthritis Care & Research (Dec. 3, 2013). The study found that about half as many people were considered disabled after the first four years of RA treatment in 2011, compared to 1990. The study analyzed data on 1,151 people diagnosed with RA between 1990 and 2011 between the ages of 17 and 86 years old. When assessing patients diagnosed with RA in the 1990s, more than 50 percent had significant disability. In contrast, only 31 percent were disabled four years after diagnosis in 2011. The improvement in rates of disability corresponded with the advent of potent biologic medications for RA, which has been shown to slow or prevent disease progression.
To continue reading this article or issue you must be a paid subscriber.
Sign in