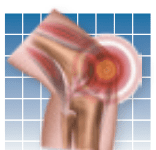
Australian researchers have found only minimal evidence that antidepressants relieve pain or depression in patients with chronic lower back pain (LBP). They did note, however, that "severely" depressed patients with LBP may still benefit from antidepressants. The findings involved a review of 10 studies published in the 2008 Cochrane Database of Systemic Reviews. The review compared antidepressants with placebo among patients [IMGCAP(1)]with LBP who were taking one of several types of antidepressants, including selective serotonin reuptake inhibitors, tricylic antidepressants, and atypical antidepressants such as aminoketone. Some medical experts who reviewed the study did not agree with the findings, claiming evidence still supports the belief that tricyclics are "moderately" effective for decreasing chronic LBP and calling for larger studies, longer-term follow-up, and an examination of the cost-effectiveness of antidepressants in treating chronic lower back pain.
To continue reading this article or issue you must be a paid subscriber.
Sign in